Introduction
Platelet-rich plasma, or PRP, is often mentioned outside of the medical field due to its increasing popularity in social media and endorsements by celebrities. Often, these people are referring to a procedure known as the “vampire facial,” which may look scary, but offers many benefits to the skin and hair. The dermatological benefits of PRP are extensive and not limited to just the face – the treatment can be used on various surfaces of the body. Studies examining the effects of PRP in various applications have documented relatively robust positive results. This blog post will outline the basics behind the PRP procedure, and how it is used to treat skin conditions like scarring, hair loss, and thinning hair.
What is Platelet-Rich Plasma?
Blood is composed of red blood cells, white blood cells, and platelets, all of which have important roles in our physiology. Platelets are of interest because they possess properties that are behind the success of these dermatological treatments. These cells are involved in blood clotting and wound healing. In addition, platelets also contain alpha-granules, which contain growth factors such as vitamins and hormones, as well as proteins, all of which can contribute to tissue rejuvenation. The secreted components interact with the local environment and stimulate processes such as cellular differentiation (one cell becoming a different type of cell), cellular proliferation (increasing cell numbers), and cellular regeneration (cells renewing themselves). (1,2)
The plasma fractions containing all of these therapeutic cell stimulants used in PRP procedures have a 3 to 7-fold higher concentration of platelets compared to whole blood.(3) The plasma serum is specially processed before use so that the beneficial components of platelets are not secreted prematurely and so the sample doesn’t clot. Ultimately, the procedure is safe with minimal side effects and contraindications, which has allowed it to carve out a niche in a wide array of dermatologic procedures. (4) This is due to the fact that the patient’s own blood is used rather than an exogenous chemical or filler, and the procedure is performed by a licensed medical professional. The multifactorial benefits and anti-inflammatory effects of PRP play roles in activation of key cell signaling pathways, like the protein kinase B pathway, through which PRP promotes hair growth and hair follicle survival. (5,6) The anti-inflammatory properties help reduce redness and swelling at injection sites when treating conditions like hair loss or acne scarring.
PRP for Skin Rejuvenation
Acne is a chronic condition that affects about 90% of people, with scarring occurring in 95% of those affected. The more severe acne is, the harder it can be to deal with physically and emotionally – it can be painful and tender, and a cause of low self-esteem and depression in many people. (7,8) As such, people go to various lengths to rid themselves of acne. Common treatments include retinoid creams, chemical peels, microdermabrasion, and laser resurfacing, all of which induce new collagen formation and remodeling, eventually improving skin texture and scar appearance. (9–11) PRP is a new option in improving the appearance of scars because it increases the density of collagen fibers, leading to the smoothing out of pitted acne scars by “filling in” the holes, overall improving the appearance of the skin. (12,13)
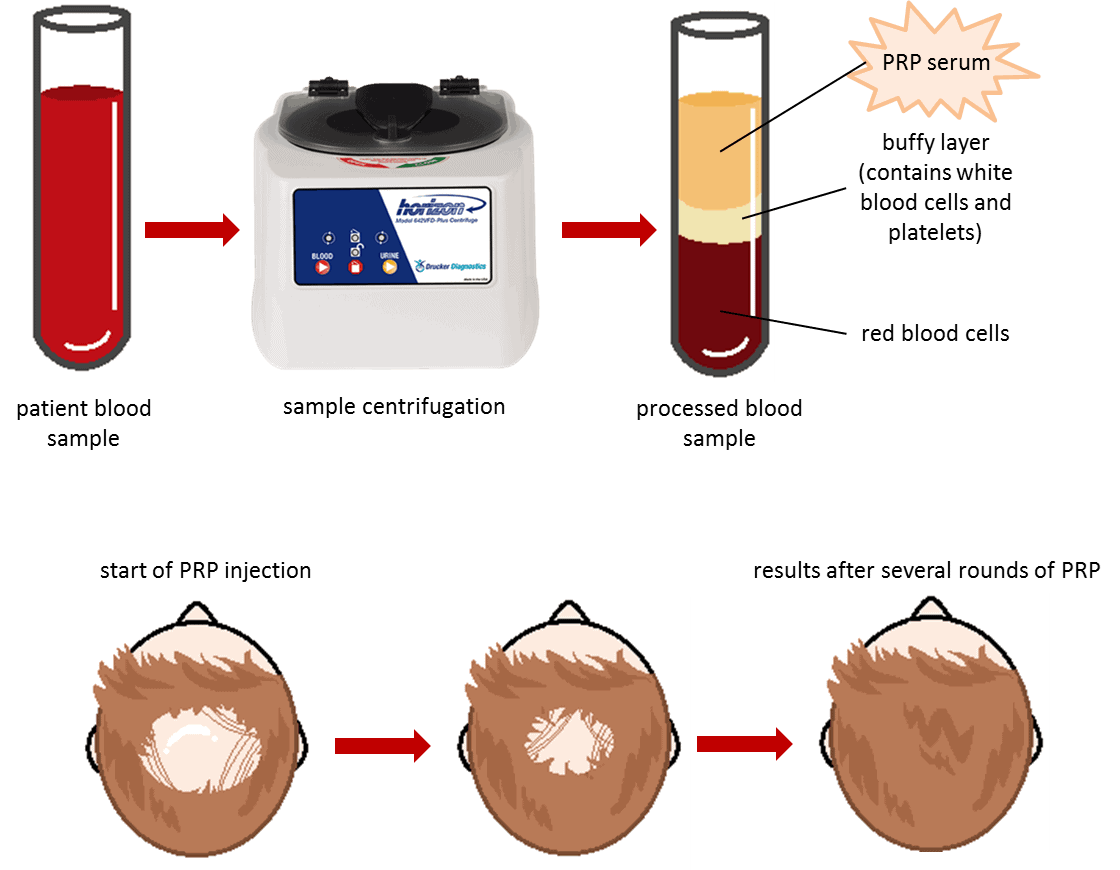
In terms of preparing PRP, the process involves an initial assessment of the face and then collecting a small amount of blood (10-60 mL) from the arm on the day of the treatment – similar to what would happen at a standard lab blood test. Anti-coagulants are immediately added to prevent the blood sample from clotting or the growth factors from activating before it is ready to be used. Centrifugation is used to process the blood sample – this entails spinning the blood sample at a very high speed, which results in the separation of the various blood cell types into distinct layers based on their weights. (3) This makes the PRP layer clearly visible and easily extracted with a syringe. In patients with healthy skin, the treatment itself consists of cleansing the face and applying a numbing cream in preparation for the microneedling pen. This tool is rolled over the facial skin to create tiny holes, which act somewhat like channels for the PRP serum and allow it to better penetrate the skin. Additionally, the creation of these holes induces collagen formation and restructuring. The PRP serum is applied over the skin. Coupled with the collagen stimulation, patients see an improved smoothness of the skin and decrease in wrinkles and scarring due to the increased wound healing response. (14–16)
The described method is usually sufficient to improve the skin’s appearance for those with mild acne scarring. (17,18) In cases of more severe acne and scarring, PRP can be injected intradermally (between skin layers) as well as microneedled and topically treated with PRP serum. Thus, the PRP works from the inside out and its benefits are localized to the injection site, reducing inflammation and improving the appearance of scars through collagen production. Although several studies demonstrate the benefit of PRP to acne scars, there is benefit to understanding how effective PRP is in different patient types – those with severe scarring, different types of scars, and scars that have varying durations. (3,19–21)
Replenishing Thinning Hair and Hair Loss
Hair loss occurs for a variety of reasons, though the most common reason is due to a genetic condition known as androgenetic alopecia (AGA). This is known as male and female pattern hair loss. AGA is one of the most common hair loss disorders and mainly affects men. (22) Although it is mostly a genetic condition, factors such as diet, stress, hormones — particularly DHT or testosterone, which strangely only affects the front and top of the head! Certain medications can contribute to its onset as well. Losing hair is actually a normal daily occurrence, and we lose upwards of 100 strands of hair daily! The problem with AGA is that the hair does not grow back, and this can understandably cause significant emotional and psychological distress as hair is one of our aesthetic defining features. (23)
Often, people will use products such as Rogaine (Minoxidil) to try to regrow their hair or thicken it, or Propecia (Finasteride) to prevent hair loss in the first place. Sometimes, people choose to undergo hair transplant surgery. Hair is grafted from the back of the head to the front through follicular unit transplantation (FUT) or follicular unit extraction (FUE). Although the results can be significant, the procedures take several hours and require downtime post-surgery. If patients have extensive AGA, more than one session may be required in order to achieve their desired aesthetic.
The biological properties of PRP are localized to the areas of the scalp where hair growth and follicle survival are desired. In addition, the anti-inflammatory effects of PRP reduce inflammation caused by AGA and PRP promotes growth and follicle survival due to the activation of cell survival factors leading to an increased viability and therefore greater number of active hair follicles. (22,24,25) The injections also stimulate natural hair growth and maintenance because they increase blood supply to the follicle, thus increasing the thickness of the hair shaft. The procedure itself is very similar to what is done in facial rejuvenation. A blood sample is drawn and processed through centrifugation to separate the components of the blood into distinct layers. Finally, the platelet rich plasma layer is injected subdermally or subcutaneously into the scalp.
Randomized controlled trials of PRP have shown that regular PRP injections can y improve hair density, count, diameter, and shedding, but the results are better in patients with mild AGA or recent onset of hair loss. This is still a new field and there are inconsistencies among measurement and protocols – as such, the comparisons made between studies are somewhat limited. PRP can also be combined with other treatment modalities to increase the robustness of results – for example, combination therapy with Rogaine, low level laser therapy, or Propecia/Finasteride can help maximize hair loss stabilization and hair regrowth. (22,23) Simply put, larger trials exploring PRP as a treatment modality compared to drugs and lasers may help determine the extent of PRP efficacy.
Conclusions
Many studies show that PRP is an effective treatment in patients with acne scarring and those with hair loss. However, it should be noted that the improvements are more robust when scarring and alopecia severity is lower, so prospective patients should always discuss their desired outcomes with their dermatologist at the initial consultation in order to manage expectations appropriately. PRP has potent healing and anti-inflammatory properties, increases hair count and thickness with minimal side effects.
References
1. Davì G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med. 2007 Dec 13;357(24):2482–94.
2. Rozman P, Bolta Z. Use of platelet growth factors in treating wounds and soft-tissue injuries. Acta Dermatovenerol Alp Pannonica Adriat. 2007 Dec;16(4):156–65.
3. Hesseler MJ, Shyam N. Platelet-rich plasma and its utility in the treatment of acne scars – A systematic review. J Am Acad Dermatol. 2019 Feb 8;
4. Anitua E, Pino A, Jaén P, Navarro MR. Platelet rich plasma for the management of hair loss: Better alone or in combination? J Cosmet Dermatol. 2018 Jun 14;
5. Sadick NS, Callender VD, Kircik LH, Kogan S. New Insight Into the Pathophysiology of Hair Loss Trigger a Paradigm Shift in the Treatment Approach. J Drugs Dermatol JDD. 2017 Nov 1;16(11):s135–40.
6. Li ZJ, Choi H-I, Choi D-K, Sohn K-C, Im M, Seo Y-J, et al. Autologous platelet-rich plasma: a potential therapeutic tool for promoting hair growth. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2012 Jul;38(7 Pt 1):1040–6.
7. Stathakis V, Kilkenny M, Marks R. Descriptive epidemiology of acne vulgaris in the community. Australas J Dermatol. 1997 Aug;38(3):115–23.
8. Goulden V, Stables GI, Cunliffe WJ. Prevalence of facial acne in adults. J Am Acad Dermatol. 1999 Oct;41(4):577–80.
9. Harris DW, Buckley CC, Ostlere LS, Rustin MH. Topical retinoic acid in the treatment of fine acne scarring. Br J Dermatol. 1991 Jul;125(1):81–2.
10. Spencer JM. Microdermabrasion. Am J Clin Dermatol. 2005;6(2):89–92.
11. Lee JB, Chung WG, Kwahck H, Lee KH. Focal treatment of acne scars with trichloroacetic acid: chemical reconstruction of skin scars method. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2002 Nov;28(11):1017–1021; discussion 1021.
12. Abuaf OK, Yildiz H, Baloglu H, Bilgili ME, Simsek HA, Dogan B. Histologic Evidence of New Collagen Formulation Using Platelet Rich Plasma in Skin Rejuvenation: A Prospective Controlled Clinical Study. Ann Dermatol. 2016 Dec;28(6):718–24.
13. Elghblawi E. Platelet-rich plasma, the ultimate secret for youthful skin elixir and hair growth triggering. J Cosmet Dermatol. 2017 Sep 8;
14. Fitzpatrick RE, Rostan EF. Reversal of photodamage with topical growth factors: a pilot study. J Cosmet Laser Ther Off Publ Eur Soc Laser Dermatol. 2003 Apr;5(1):25–34.
15. Mehta RC, Smith SR, Grove GL, Ford RO, Canfield W, Donofrio LM, et al. Reduction in facial photodamage by a topical growth factor product. J Drugs Dermatol JDD. 2008 Sep;7(9):864–71.
16. Atkin DH, Trookman NS, Rizer RL, Schreck LE, Ho ET, Gotz V, et al. Combination of physiologically balanced growth factors with antioxidants for reversal of facial photodamage. J Cosmet Laser Ther Off Publ Eur Soc Laser Dermatol. 2010 Feb;12(1):14–20.
17. Fabbrocini G, De Vita G, Pastor FJ, Panariello L, Fardella N, Sepulveres R, et al. Combined use of skin needling and platelet-rich plasma in acne scarring treatment. 2011;24:117–83.
18. Nofal E, Helmy A, Nofal A, Alakad R, Nasr M. Platelet-rich plasma versus CROSS technique with 100% trichloroacetic acid versus combined skin needling and platelet rich plasma in the treatment of atrophic acne scars: a comparative study. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2014 Aug;40(8):864–73.
19. Asif M, Kanodia S, Singh K. Combined autologous platelet-rich plasma with microneedling verses microneedling with distilled water in the treatment of atrophic acne scars: a concurrent split-face study. J Cosmet Dermatol. 2016 Dec;15(4):434–43.
20. Ibrahim ZA, El-Ashmawy AA, Shora OA. Therapeutic effect of microneedling and autologous platelet-rich plasma in the treatment of atrophic scars: A randomized study. J Cosmet Dermatol. 2017 Sep;16(3):388–99.
21. El-Domyati M, Abdel-Wahab H, Hossam A. Microneedling combined with platelet-rich plasma or trichloroacetic acid peeling for management of acne scarring: A split-face clinical and histologic comparison. J Cosmet Dermatol. 2018 Feb;17(1):73–83.
22. Gupta A, Carveil J. A Mechanistic Model of Platelet-Rich Plasma Treatment for Androgenetic Alopecia. Dermatol Surg. 2016;42(12):1335–9.
23. Tabolli S, Sampogna F, di Pietro C, Mannooranparampil TJ, Ribuffo M, Abeni D. Health status, coping strategies, and alexithymia in subjects with androgenetic alopecia: a questionnaire study. Am J Clin Dermatol. 2013 Apr;14(2):139–45.
24. Mahé YF, Michelet JF, Billoni N, Jarrousse F, Buan B, Commo S, et al. Androgenetic alopecia and microinflammation. Int J Dermatol. 2000 Aug;39(8):576–84.
25. Magro CM, Rossi A, Poe J, Manhas-Bhutani S, Sadick N. The role of inflammation and immunity in the pathogenesis of androgenetic alopecia. J Drugs Dermatol JDD. 2011 Dec;10(12):1404–11.