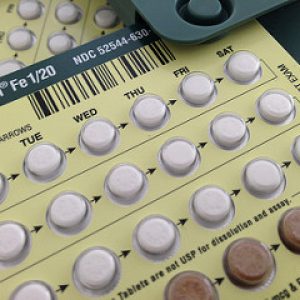
As mentioned in part 1 of this mini-series, birth control pills have the potential to promote hair loss or hair gain. The likelihood of each option depends on multiple factors including the combination of hormones in your particular brand of pill and your own body characteristics.
Hormones are an essential part of many of the processes taking place throughout the body. Androgens are hormones which can lead to the development of body and facial hair, oily skin, acne and pattern baldness. An overabundance of androgens can sometimes lead to androgenisation, which may result in any of the above symptoms, or a diagnosis of polycystic ovary syndrome (PCOS) is also possible1. Likewise birth control containing hormones with androgenic properties can promote these symptoms such as hair loss2.
Alternatively, there are birth control options which contain hormone combinations that result in anti-androgenic properties1,3. By suppressing the effects of naturally present androgens, some hormone combinations can encourage hair growth and are used to treat androgenisation1. Anti-androgenic birth control such as options that contain progesterone in the form of drospirenone and estrogen in the form of ethinylestradiol are examples that can lead to hair gain1.
The downside to these types of birth control pills is that they come with a higher risk of serious side effects including blood clots. Health Canada estimates that the risk is 1.5 to 3 fold higher than that of other types of birth control pills; however the overall risk is still small and lower than that associated with pregnancy4–8. Those who smoke, struggle with obesity or have a family history of blood clots may be at a higher risk for serious side effects.
Taken together, the choice to use the pill as contraception can be a substantial decision. There are many benefits but you should also clearly understand any potential side effects. Your doctor can help to assess your individual situation.
Article by: Dr. J.L. Carviel, PhD, Mediprobe Research Inc.
References
- Schindler AE. Antiandrogenic progestins for treatment of signs of androgenisation and hormonal contraception. Eur J Obstet Gynecol Reprod Biol. 2004 Feb 10;112(2):136–41.
- Teichmann AT. [Rationale for prescribing oral contraceptives]. Wien Med Wochenschr 1946. 1998;148(7):171–4.
- Schindler AE. Non-contraceptive benefits of hormonal contraceptives. Minerva Ginecol. 2010 Aug;62(4):319–29.
- Lidegaard Ø, Løkkegaard E, Svendsen AL, Agger C. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:b2890.
- Parkin L, Sharples K, Hernandez RK, Jick SS. Risk of venous thromboembolism in users of oral contraceptives containing drospirenone or levonorgestrel: nested case-control study based on UK General Practice Research Database. BMJ. 2011;342:d2139.
- Jick SS, Hernandez RK. Risk of non-fatal venous thromboembolism in women using oral contraceptives containing drospirenone compared with women using oral contraceptives containing levonorgestrel: case-control study using United States claims data. BMJ. 2011;342:d2151.
- Vinogradova Y, Coupland C, Hippisley-Cox J. Use of combined oral contraceptives and risk of venous thromboembolism: nested case-control studies using the QResearch and CPRD databases. BMJ. 2015;350:h2135.
- van Hylckama Vlieg A, Helmerhorst FM, Vandenbroucke JP, Doggen CJM, Rosendaal FR. The venous thrombotic risk of oral contraceptives, effects of oestrogen dose and progestogen type: results of the MEGA case-control study. BMJ. 2009;339:b2921.












